How do you go about getting work experience in the medical field. If theres one complaint that is chanted in unison by aspiring medics – It’s that getting work experience is one of the hardest aspects of the application to acquire. However with just some thinking outside the box, your chances of getting work experience can be greatly improved.
I have applied to many “trusts” for work experience in NHS hospitals, like John Radcliffe, and Stoke Mandeville Hospital, however have been unsuccessful in getting any responses from these trusts. Now it makes sense right, the NHS is under heavy pressure to relieve many millions of backlogs of patient appointments, their staff might just not have enough time to give to teach or allow aspiring medics to work shadow them. Even if someone may get a place at one of these trusts for work experience, I have heard from my friends that there was not much explanation of what was going on, or why a doctor was doing something. It was almost like they felt like an isolated spectator in the hospital, which is not really beneficial, because medical schools don’t just want you to have work experience, they want you to be able to reflect on what you learnt from it and took away from the whole experience. If you weren’t able to learn anything or understand, then it’s safe to ask what was point of it.
So my thought process went as follows; If the NHS is very busy and does not currently have the time to help me as an aspiring medic, then hopefully the private medical sector would be able help me. To my surprise, I was very much correct. After calling the reception of Royal Buckinghamshire Hospital, I was quickly directed to an email that I was asked to email with details regarding my work experience. I got a response very quickly – within a day, and within 2 days I was already meeting with Mohammad from the Hospital. This rapid response time was very much to my surprise.
It was very nice speaking to Mohammad on the first day of work experience. When I was asked the question “So when can you start”, I said giddily “I can start from today”, as we sit in a massive conference room at 8:30 in the morning. What I hoped to gain from this work experience was an overview of the entire process of Patient admission to discharge, software and communications that nurses use, ward rounds and clinical rounds, medicine dispensary, and hospital asset management and procurement. So Mohammad suggested that I spend a day with each department, and shadow them, so that I can have a nice overview of all of the departments and have a wide taste of how every department works both in isolation and in synergy.
Introduction to the Therapy Department
My first day started off in the Therapy Department, along with an introduction to the department head – Hayden. Deborah took me on a quick tour of the therapy rehab premises and gave me a rapid fire naming of all of the equipment that they had in stock:
- Hoist
- Functional Electrical Stimulation
- Transfer Equipment
- Anti-Gravity machine
- Exoskeleton Machine
- Saebo arms
- Laser equipment (kLaser)
- Xbox/Wii U
- Pressure Cushions
- Transfer Board
- Upper limb FES bike
- Stim
- Quad Stick
- Pool – Hydrorehab
This was a rapid fire session which was just before a goal setting meeting between the entire therapy department.
Goal Setting
Goal setting was a very unique and interesting meeting to me, as it included setting and updating specific goals for therapy rehab patients. I will only talk about patients with attributes so that they are not able to be identified due to doctor-patient confidentiality. For example Patient X had the following goals:
- Needs help to be fully independent with all functions of living.
- To be independently managing all of their daily needs.
- To be able to stand up from the floor with assistance of 1 person.
- To be able to mobilise on the treadmill at speed 2 for 30 minutes with 70% of their weight.
- To be able to independently access the community with their 4-wheeled walker.
These goals can then be classified with not achieved, ongoing, achievable, and achieved, along with a timeframe of approximately when the therapy specialists think the patient will be able to fully achieve the goal by. This collaboration between all of the specialists to ensure that a patient had correct and appropriate goals was very interesting to me, because it showed me how in healthcare it is important to be able to work seamlessly with the multidisciplinary team.
Another interesting thing to hear during this meeting was how 2 occupational therapists shared their experiences with a specific patient X. During the discussion, occupational therapist A informed occupational therapist B that Patient X was getting too reliant on Therapist B’s presence to do her activities and sessions, hence a suggestion was put forward to vary the specialist that was working with Patient X more often, so that the patient did not develop too much of a reliance and connection with a specific rehab therapist. However working with multiple different specialist therapists can actually be one of the benefits of coming to a Private Hospital to get treatment, because if one therapist’s methods are not working and are not being successful, then at least another specialist’s techniques might be able to make progress with the patient. However if there is only one therapist specialist and they get stuck while making progress with a patient, then the patient will also be stuck, and unable to progress further.
Another example of patient goals are as follows for patient Y:
- To be able to reach forwards with right upper limb and grasp a target (2 weeks)
- To be able to step transfer with a zimmer frame and assistance of 1 person (2 weeks) -> 50 meters for today.
- To be able to maintain right knee extension in stance phase of gait (2 weeks).
- To be able to use a keyboard with both hands (4 weeks).
- Goals for cooking, and making a cup of tea.
Once the goal setting meeting was concluded, Hayden ensured that I was aware of the timetable for the whole day, and circled on the timetable the sessions that I could attend, which would allow me to view the widest range of devices used, and medical conditions.
Patient Sessions
Lets jump straight into the first session/ patient meet. Instantly I take note of how the specialist was communicating with the patient, as I realise the specialist is trying to build a rapport with the patient, but this time I can observe how they are able to achieve this, rather than just seeing it copy-pasted everywhere online as a key piece of advice for MMI’s. To begin with the specialist is asking the patient what they did yesterday, and if they remember what their session consisted of yesterday. Unfortunately the patient did not have such a positive outlook and mindset, instead replying with something along the lines of “I want to give my leg away”. This patient has a foot defect, where her ankle and foot are curving inwards at a sharp angle. This definitely causes the patient a lot of pain, but there are various methods that are taken to reduce the pain that the patient is feeling.
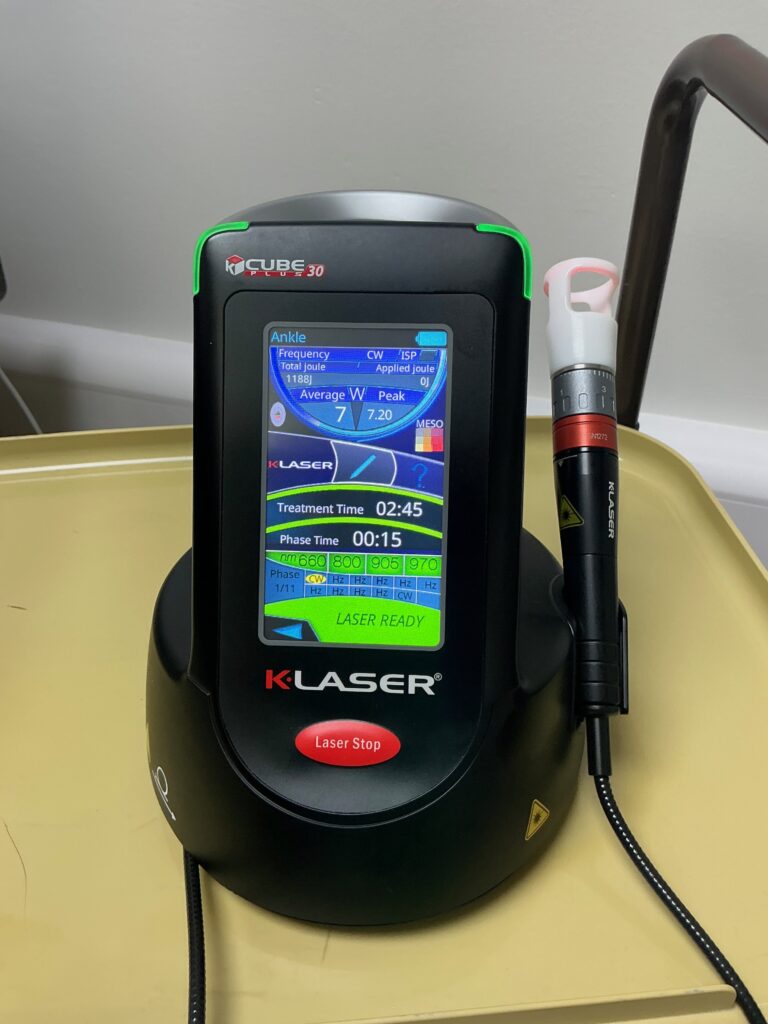
For example I observed the usage of the KLaser, which has settings to change the wavelengths and frequency it emits. The usage of the KLaser is to reduce pain, and induces anti-information and anti-inflammation in a limited section of soft tissue. While a painkiller like paracetamol goes through the blood stream to reach where it needs to go to numb the pain, the KLaser is very localised, so is very effective and quick. Also, while paracetamol will spread out over the blood stream, KLaser will have faster and more impressive results. However this quick and rapid pain relief does not come cheap for the hospital. A little device like the once shown below costs anywhere upwards of £40,000.
Another patient was stimulated to stand momentarily with the help of a MoLift. A MoLift is usually used for patient transfer, but in this case can also be used to stimulate someone to stand.
During my time at the hospital I also learnt some terminology. For example paraplegic patients have no control of any of the lower limbs. MoLift cannot be used to help any patients with zero control of the lower limbs. They must have at least some control of even one half of the lower limbs. The reason for Molift/this is because if there are limited muscles/atrophied muscles in the legs, then under standard pressure of the patient trying to walk, there will be 50kg-60kg on only 1 leg/knee ligaments, which is not built to be having so much pressure, so there is an increased chance of it snapping. This is mainly because the knee is not meant to hold such amounts of force on itself.
The hospital also has a pool, which can be used for hydro-rehab. This works extremely well because there is a 360 degree field of movement for the patient, which allows them more freedom of movement than perhaps say a MoLift, or something like an exoskeleton. While the water also adds a layer of resistance to the movement, which helps atrophied muscles regenerate at a faster rate, because of the extra pressure/strain that the patient is using to move them. This was very striking and interesting to hear the use of, because it is the first time I had heard of a pool being used in a hospital.
I also saw another patient meet/session. This was a patient with a cognitive defect, and they were in a wheelchair. Again I was able to see how the healthcare specialist was able to build a rapport with the patient, again by asking the patient simple questions, like how did they sleep yesterday, and if they are tired right now. If there was one thing to take away from this, it was the sheer amount of energy that was radiating from the healthcare specialist. In their voice, there was a sense of playfulness and not too serious. I was able to see a great example of problem solving in this session, where the patient was not responding to the task at hand, which was picture matching cards. Hence the occupational therapist changed the task to get more of a response out of the patient, by showing the patient pictures from their childhood. This worked better to at least get a response out of the patient, and hence likely stimulated the patient’s cognitive abilities more than if the occupational therapist just kept on pushing with the picture matching game. The occupational therapist also was able to attract the patients eyes and focus back to them, even though the patient was getting distracted by other noises and sounds in the ward. In conclusion the patient was responding better to questions when looking at pictures that reminded him of a memory and a good past.
There was also another patient who was suffering from a stroke. They had paralysis in the whole of the right hand side. The patient has goals to travel with a quadstick and zimmer frame, goals that were discussed during the goals setting meeting at the start of the day. This patient had 4 sessions a day, which is the maximum any patient can have per day. This is good because it shows how determined the patient is towards their own success. After-all rehab is a certain branch of medicine where the healthcare professionals are not the only ones putting in the effort for a better patient outcome, the mindset and effort that the patient puts in can also go a long way towards helping their own outcome. Unfortunately this patient was telling me that there was a 6 week period directly after having a stroke that they were unable to have any movement. They are able to feel sensations/skin touch on the right hand side, but cannot move feely. Stroke affected the left side of the brain, so the right hand side of the body is affected. Retraining the brain to allow usage of the body limbs is called neuroplasticity, which is retraining neural pathways that have been forgotten about or broken. One of the goals of this patient was to do a pivot transfer from his wheelchair to a stool, and I’m glad to say that this patient was able to achieve this goal within 3 days. The first time I saw the patient was on thursday, and on Monday they were able to do a full pivot turn without any help from the healthcare therapists. The patient after receiving an oil massage on his arms, which helps with pain relief, then moved to use the My Motion Go machine. It is a machine that is connected to a computer. There is a tool to check the grip strength of the patient. Using the saebo arm to ensure the patient can keep his On the computer screen there is a hot air ballon game, where the hot air balloon goes up and down based on the grip firmness that the patient exerts on the hand grip tool. Then the patient played a game where the input of the machine was moving his hand left to right. This was to stimulate both up and down and left to right movement of his arm, again referring to the term of neuroplasticity. Machine called a tyrostation.
Grand Round
The grand round was also an impressive thing I was able to observe. It was a meeting between many department heads (Occupational therapy, Physiotherapy, Diabetics, Nurse, Doctor) to discuss each patient the hospital had. The meeting took place in a large conference room with plushy chairs, an 8k tv screen, with a pc connected to it, and a Logitech ultra-wide angle webcam. The way the grand round works is a word document gets updated which everyone in the conference room can see, as well as the pharmacist, and other staff on a Teams call. The word document had boxes for each department pertaining to each patient. So for example patient X would have boxes for notes from the following: Nursing, Medical/Pharmacy, Dietary, Speech and Language therapy, Physiotherapy, Occupational Therapy, Psychological, Patients feelings/confidence in treatment. There were also notes about where the patient would stay, before their admission to the hospital, or after their admission to the hospital. Each of the heads of department give their own opinion on how they feel the patient is doing.
The experience was an eye-opener to how much teamwork, thought, and care goes into every step of the patient’s recovery. It taught me that healthcare is about adapting, collaboration, patience, and creativity.

No responses yet